How to pass the FDA Refusal to Accept (RTA) Screening Process
This article helps you understand how to pass the FDA Refusal to Accept (RTA) screening process 510k submissions – updated April 2022.
What is an RTA Checklist?
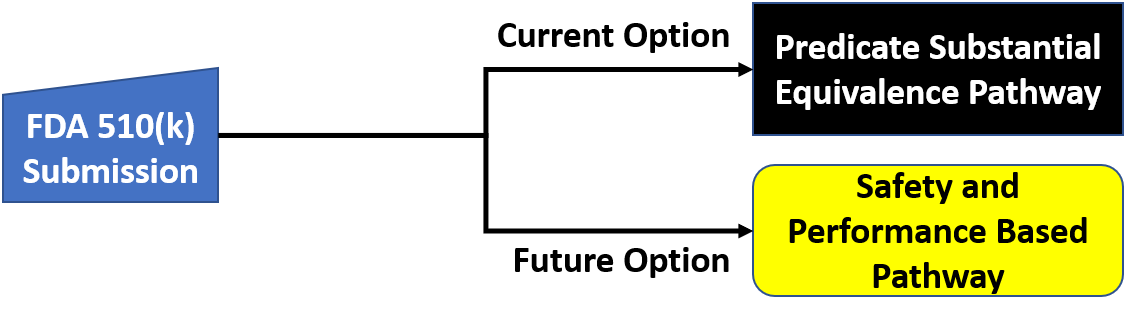
The “RTA” in RTA Checklist stands for Refuse to Accept. The FDA uses this tool to determine if your 510(k) submissions will be accepted or not for a substantive review. Accepted, not approved because this is simply a verification that the required information is included in your submission. As stated in the 2022 FDA guidance document for the FDA’s Refuse to Accept Policy for 510(k)s “a minimum threshold of acceptability and should be accepted for substantive review.”(Ref.1). That does a nice job summarizing the RTA checklist. It is a tool used to help assess whether or not your submission contains the required information to continue with a more thorough review of the contents of the submission itself.
What does the Refusal to Accept (RTA) policy apply to?
The Refusal to Accept (RTA) policy applies to all 510k submissions. The RTA checklist or more checklists apply specifically to each 510(k) submission type:
- Traditional 510k
- Abbreviated 510k
- Special 510k
There is a different RTA checklist for each submission type. The checklists are in the Refuse to Accept Policy for 510(k)s guidance document. Specifically, in the PDF document that the FDA reissued in April 2022, the checklists can be found in the following areas:
- Traditional 510k – Appendix A.
- Abbreviated 510k – Appendix B.
- Special 510k – Appendix C.
Note that the title of the checklist refers to an ‘acceptance checklist.’ It is not called the RTA checklist until you get to the footer of the page. It is also listed as an acceptance checklist on the FDA website. The best way to think of the process is as preliminary screening by the FDA.
What does the FDA look at during the Refusal to Accept (RTA) screening process?
During the screening process, the assigned RTA screener will review the 510k submission and try to identify all of the requirements listed in the applicable RTA checklist. The person screening your submission is required to answer “yes,” “no,” or “n/a” to the questions in the checklist. This person must also enter the document and the page where the information can be found in the submission. Finally, if an element required by the refusal to accept (RTA) checklist cannot be found, then the screener adds a comment at the end of that section in the checklist. The comment will state what your deficiency is and it may even identify a guidance document that can help you address the issue. If you are missing requirements, you will receive an email from the RTA screener with the completed RTA checklist attached. We call this an “RTA Hold” letter. If your submission is not rejected, then your 510k is administratively complete, and you will receive an automated email indicating that your submission was accepted and the substantive review will begin.
Refusal to Accept (RTA) Time Frame
As stated in the guidance document, the Refusal to Accept policy includes “an early review against specific acceptance criteria and to inform the submitter within the first 15 calendar days after receipt of the submission if the submission is administratively complete, or if not, to identify the missing element(s).” (Ref. 1). If the assigned screening person is unable to complete the process within 15 calendar days, then you will receive an automated email stating that they were unable to complete the RTA checklist within 15 calendar days, and your submission is automatically moved to the substantive review stage of the 510k review process.
Taking the time to perform your gap analysis before submitting could avoid a simple error. For example, if you forget to include the signed Truthful and Accuracy Statement in your submission, it could take 15 days to be notified of that missing element. The person screening your submission could email you to provide this missing element in an interactive review to avoid placing your submission on hold. Still, they are not required to give you a chance to provide this interactively by email. If you do receive an RTA Hold letter, you might be able to correct missing elements on the same day, but the 510k review clock is automatically reset when your 510k is placed on RTA Hold. When you respond to an RTA Hold letter, there will be another 15-day refusal to accept (RTA) screening of your submission.
What do you do with the information in the comments of the RTA checklist?
The RTA checklist is the criteria that your submission is being evaluated against. Suppose your submission has deficiencies during the initial review against the RTA Checklist. In that case, the FDA will refuse to accept it, and the substantive review will not begin until those deficiencies have been corrected. Since the FDA does not hide what they are looking for or how they will evaluate your submission, use that to your advantage. Assuming that you have correctly determined the type of 510k submission you have, perform a gap analysis of your submission against the RTA checklist. Either perform these actions in-house or hire an outside consultant to do them for you, but make sure you don’t try to check your own work because you will miss something.
Scope of the FDA Refusal to Accept Guidance Document
The scope of the FDA guidance document is provided for the benefit of the FDA personnel reviewing your submission and not specifically for the 510k submitter. It also provides a loose framework for systematically and consistently reviewing submissions. This ensures all submissions receive equal, nonbiased treatment. There are some things that this guidance document does not address or alter by its own admission. One is the “substantial equivalence decision-making process once the submission has been accepted for review.” Refusing to accept (RTA) guidance also does not address FDA user fees. Other guidance documents address those issues.
What are the most common reasons for FDA refusal of your 510k submission?
Although there are dozens of reasons (43 to be exact) why the FDA could reject your submission in the 35-page RTA checklist, most of the refusals (~80%) result from a small percentage (~20%) of reasons. The most common is that your submission is poorly organized. Either you did not provide a table of contents, your submission is not organized in accordance with the sections outlined in the guidance, or the pages of your submission are not properly numbered. When trying to review a 1,200-page submission, poor organization is extremely irritating and wastes the reviewer’s time. If it were my decision, I would refuse to complete the entire checklist until you gave me a properly organized submission.
The second most common reason for refusal is submitting a device description that is inadequate. The FDA needs more detail than most companies provide for the device description because they need to understand the differences between your device and the predicate device. This includes much more than just the indications for use. Who are the intended patients and users? What is the intended environment of use? What are the materials for patient-contacting components? What is the source of power for your device? Which design features does your device include when compared to the predicate? What is the user interface for your device? Which accessory devices are needed with your device? You can even make the mistake of being inconsistent in your submission by not repeating the content in the device description in other sections of the 510k submission. It is important to duplicate certain content verbatim in other documents, such as the 510k summary, the executive summary, the substantial equivalence comparison, and the instructions for use. Paraphrasing and summarizing certain information will not work.
The third most common reason for refusal of your submission is likely related to software validation documentation. In addition to complying with the recognized IEC 62304 standard, you must also comply with the five software guidance documents published by the FDA. The FDA and 3rd-party reviewers use an 11-item checklist based on the 2005 FDA guidance document on software validation documentation. In addition, if your device has any of the following five elements, your submission must also comply with the two FDA guidance documents on cybersecurity:
- Cloud communication
- Network connection (active or not)
- Wireless communication in any form
- USB/serial ports/removable media
- Software upgrades (this includes patches)
Finally, biocompatibility is the one testing section of your 510k submission that is most likely to result in refusal to accept by the FDA out of the seven sections requiring testing reports. There are several reasons why biocompatibility results in more refusals than the other six testing sections. First, the FDA requirements go above and beyond the ISO 10993-1 standard requirements. Second, the FDA requires that you submit full testing reports for biocompatibility, while you can submit summaries for other sections (e.g., sterilization validation). Third, many submitters try to provide a rationale for why testing is not required for their device. Still, the FDA has very stringent requirements for the use of a biological risk assessment or a biocompatibility certification statement in lieu of testing.
Do you have to follow the RTA checklist exactly?
You can, but you are also not bound by it. Like all guidance documents, they “contain nonbinding recommendations”. The checklist is released as part of a guidance document, so it is a guidance and not a regulatory requirement. That being said, if your submission is missing an element in the checklist, your 510k submission will be considered administratively incomplete unless you provide a clear explanation as to why the checklist element does not apply to your submission or you explain how you meet the 510k submission requirement in another way.
Medical devices vary wildly, and there is no one size fits all approach. The FDA recognizes that and includes some wiggle room that gives them some discretion in reviewing submissions. However, 100% of the 3,500+ submissions received each year are screened using the refusal to accept (RTA) checklist, and the screening person’s job is to verify that your submission meets the criteria. As it says in the guidance document:
“The purpose of the 510(k) acceptance review is to assess whether a submission is administratively complete, in that it includes all of the information necessary for FDA to conduct a substantive review. Therefore, the submission should not be accepted and should receive an RTA designation if one or more of the items noted as RTA items in the checklist are not present and no explanation is provided for the omission(s). However, during the RTA review, FDA staff has the discretion to determine whether missing checklist items are needed to ensure that the submission is administratively complete to allow the submission to be accepted. FDA staff also has the discretion to request missing checklist items interactively from submitters during the RTA review. Interaction during the RTA review is dependent on the FDA staff’s determination that outstanding issues are appropriate for interactive review and that adequate time is available for the submitter to provide supporting information and for FDA staff to assess responses. If one or more items noted as RTA items on the Acceptance Checklist are not present, FDA staff conducting the acceptance review should obtain management concurrence and notify the designated 510(k), contact person, electronically that the submission has not been accepted. “ (Ref. 1).
The portion above notes that explanations may be provided for omitted portions of the submission. So, the answer to the question is that no, you do not have to follow the RTA checklist exactly. However, if you should purposefully omit a section you should provide an explanation and your rationale justifying why the omission is appropriate for your individual device and 510(k) submission. Again, just because you have included an alternative approach or justification does not automatically mean it will be accepted. The FDA personnel who are conducting the acceptance review will judge whether or not your deviation is acceptable.
What if your 510k submission is refused?
If your submission is refused, you will be provided with a copy of the completed RTA checklist, and each of the deficiencies you must address will be highlighted. Sometimes, there will be an attachment to the checklist that has additional issues that are not in the RTA checklist, but the reviewer thinks you may need to address them later. You might also see comments that are not highlighted. These are suggestions from the reviewer that you may or may not choose to address.
There is a 180-day timeline for response to an RTA Hold letter. The response must be submitted to the CDRH Document Control Center (DCC) as an eCopy, and the response must be received within 180 days. If the response is not received within 180 days, your submission will be automatically withdrawn on the 181st day. Your response may not be piecemeal. You must address all of the issues in the RTA checklist or your submission will be placed on RTA Hold again (i.e., RTA2). If you are not sure how to organize your response, a previous blog posting and YouTube video address this topic directly.
About the Author
 Matthew Walker – QMS, Risk Management, Usability Testing, Cybersecurity
Matthew Walker – QMS, Risk Management, Usability Testing, Cybersecurity
Matthew came to us with a regulatory background focused on OSHA and NFPA regulations when he was a Firefighter/EMT. Since we kidnapped him from his other career, he has worked in medical device quality systems and technical/medical writing and is a Lead Auditor. Matthew has updated all of our procedures and is currently a student in Champlain College’s Cybersecurity and Digital Forensics program. We are proud to say he is also a Golden Keys and Phi Theta Kappa Honor Society member! Matthew participates in our audit team and is passionate about risk management and human factors engineering. Always the mad scientist, Matthew pairs his professional life in regulatory affairs with hobbies in the culinary arts, as he also holds a Butchers/Meat Cutters certificate from Vermont Technical College.
Email: Matthew@FDAeCopy.com
Connect on Linkedin: http://www.linkedin.com/in/matthew-walker-214718101/
How to pass the FDA Refusal to Accept (RTA) Screening Process Read More »



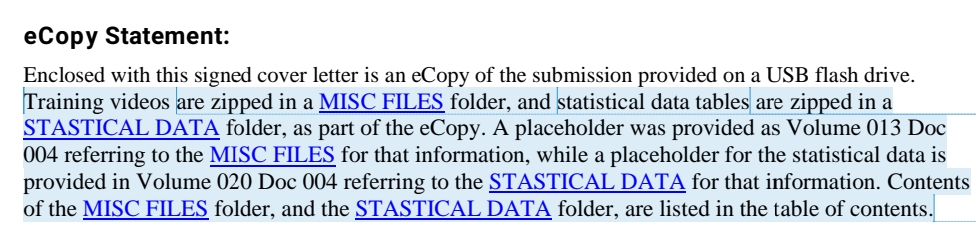

 Warning: If you are using Windows 10, and you save your eCopy or eSubmitter zip folder on a flash drive, Windows 10 will automatically create a hidden system folder titled “System Information Volume.” This folder is created as a security feature to enable you to recover accidentally deleted content. However, this folder results in an error when the FDA attempts to upload your submission automatically. Therefore, you must remove this hidden system folder. Instructions for this can be found on our website page about
Warning: If you are using Windows 10, and you save your eCopy or eSubmitter zip folder on a flash drive, Windows 10 will automatically create a hidden system folder titled “System Information Volume.” This folder is created as a security feature to enable you to recover accidentally deleted content. However, this folder results in an error when the FDA attempts to upload your submission automatically. Therefore, you must remove this hidden system folder. Instructions for this can be found on our website page about