Before 510k clearance, 10 quality tasks you need to prevent unexpected delays
The US FDA does not require that 100% of your quality system be implemented before 510k clearance, but these 10 activities need to be done.
The form above allows you to register for a live webinar we are hosting on Friday, May 21, 2021 @ 1 pm EDT. The webinar will share the 510k project management lessons learned by our team since 2016. In addition to 510k project management, MedTech companies also need to implement their quality system in parallel with their regulatory submissions. Some people say that you need to implement your quality system before you submit your 510k. That is not an FDA requirement, but you do have quality system activities that need to be done before you will have all of the technical documentation you need to submit a 510k. This article describes 10 quality tasks you need to prevent unexpected delays.
Design & Risk Management Planning
Design & Risk Management Planning is your 1st priority because you want to identify all of the major activities that need to be completed in your design and risk management processes and which activities are critical path items. Otherwise, you will have unexpected delays. You can and should add details to the plan as you go, but items 2-9 listed below should be included in that initial plan–along with your design and risk management activities.
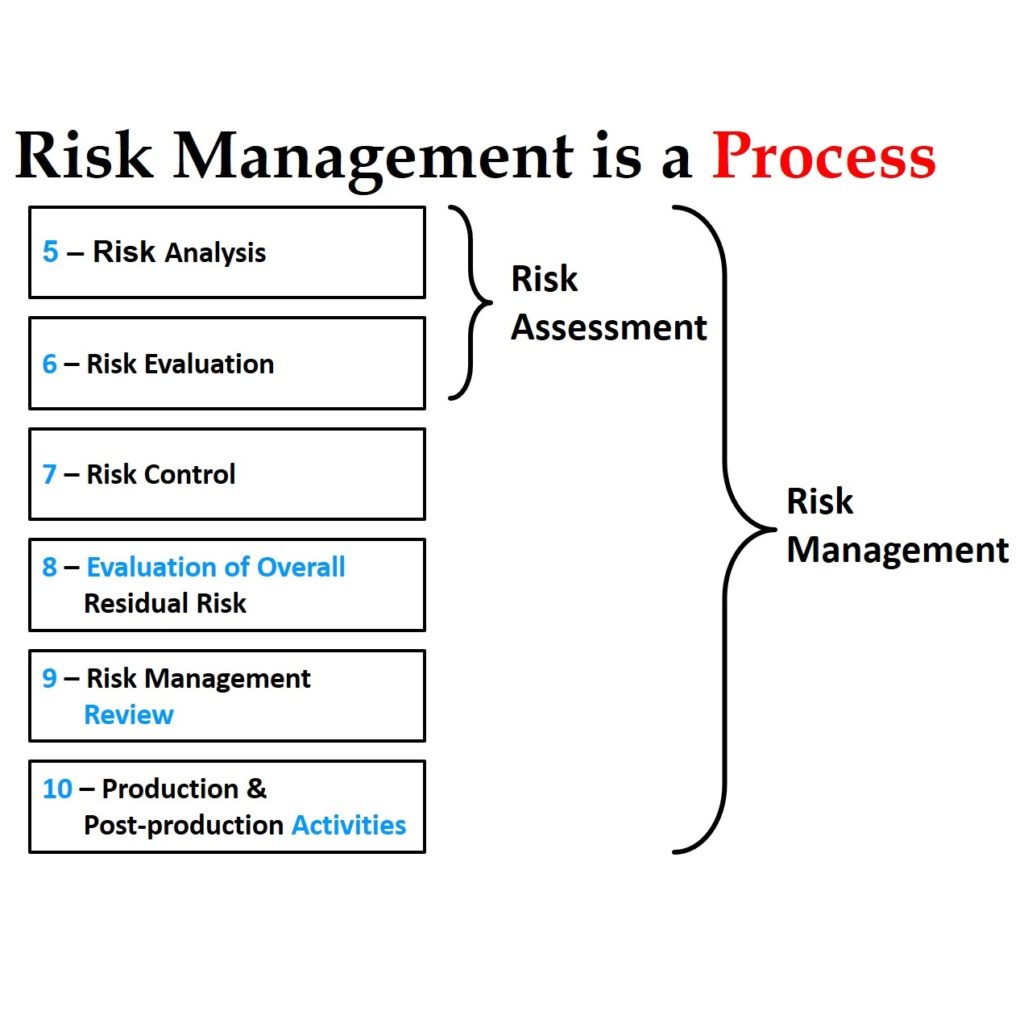
Risk Management Activities are Needed Before 510k Clearance
Risk Management is your 2nd priority because it’s an input to almost everything else listed below – this includes hazard identification, creating a use-related risk analysis (URRA), and identifying cybersecurity risks if you have software/firmware. Reference: ISO 14971:2019 Medical devices — Application of risk management to medical devices. Cybersecurity depending on the device should evaluate security as an overlapping but separate area from risk management. (Reference AAMI TIR57: 2016 Principles For Medical Device Security – Risk Management.)
Formative Usability Testing
Formative Usability Testing is your 3rd priority because this helps you evaluate your device design while it’s still evolving. Formative testing helps you identify opportunities for improvement, provides confirmation that your design is moving in the right direction, and identifies potential use errors while there is still time to implement effective risk controls such as alarms and other safety features. References:
- Applying Human Factors and Usability Engineering to Medical Devices Guidance for Industry and Food and Drug Administration Staff (2016)
- IEC 62366-1:2015 Medical devices — Part 1: Application of usability engineering to medical devices / AMD 1:2020
Software Validation is Needed Before 510k Clearance
Software Validation is your 4th priority because it must precede electrical safety testing for electromedical devices and most companies underestimate the time required to document software validation in accordance with IEC 62304:2006 / AMD 1:2015 and the FDA’s five guidance documents:
- General Principles of Software Validation:2002
- Guidance for the Content of Premarket Submissions for Software Contained in Medical Devices:2005
- Off-The-Shelf Software Use in Medical Devices:2019
- Content of Premarket Submissions for Management of Cybersecurity in Medical Devices:2014
- Postmarket Management of Cybersecurity in Medical Devices:2016
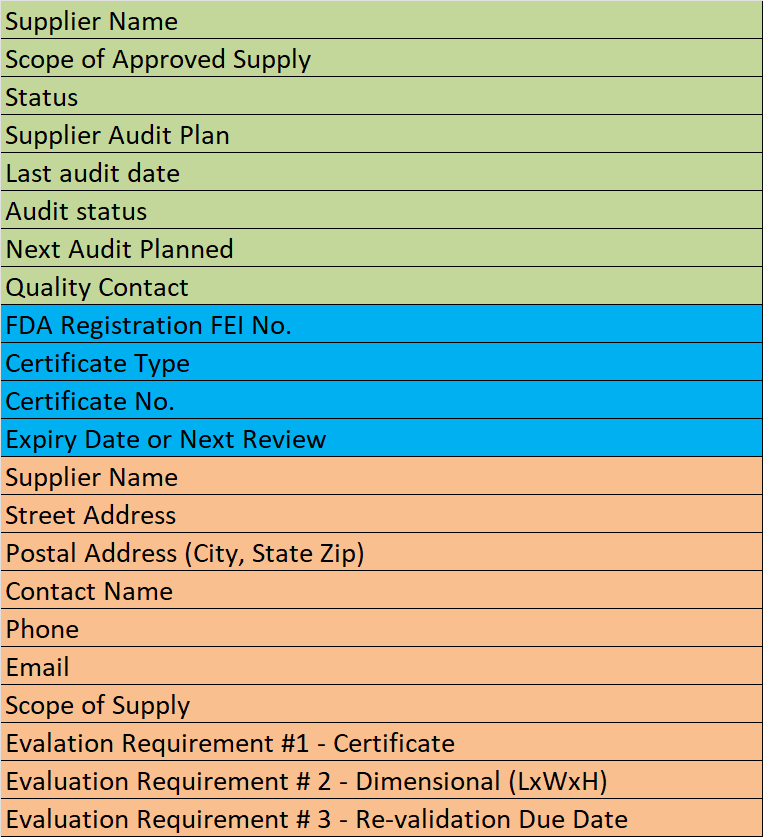
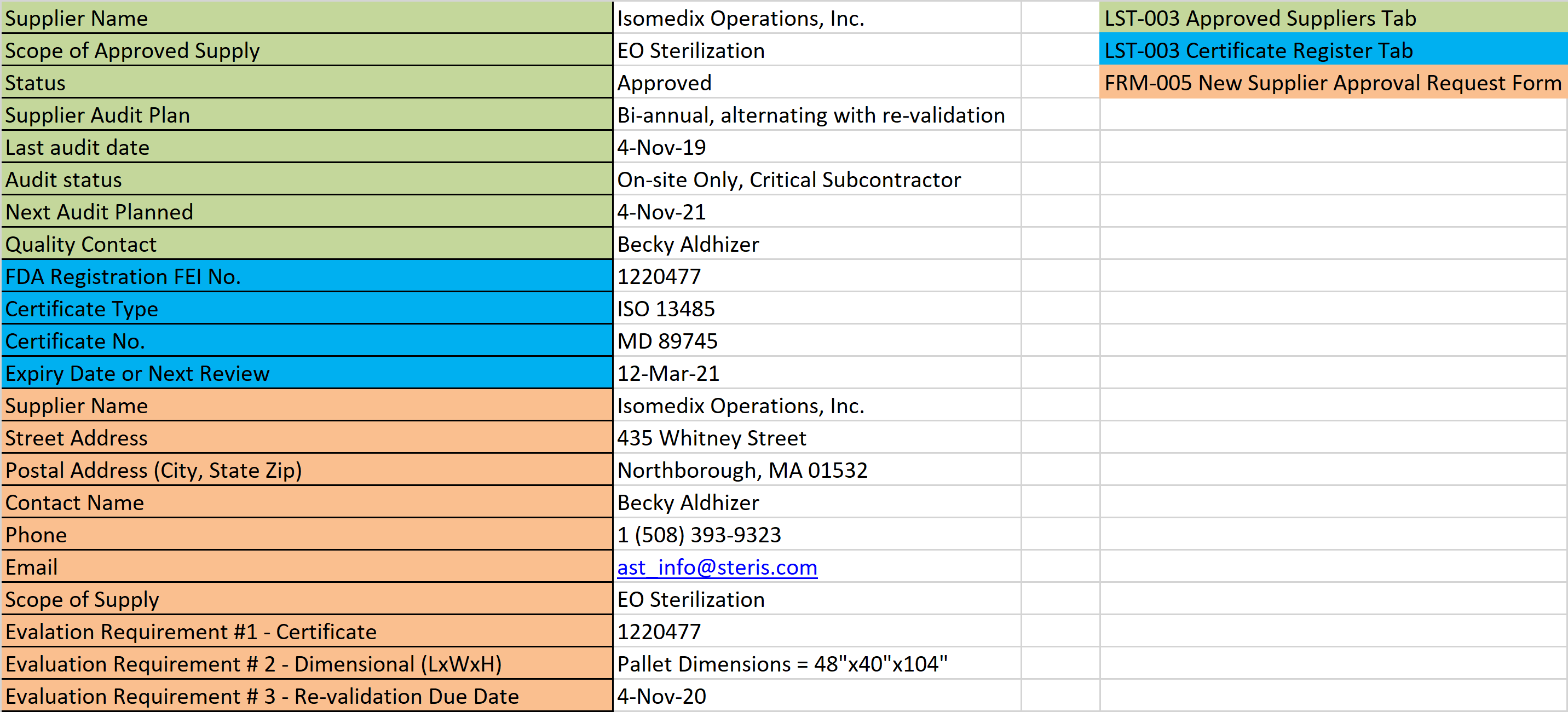
Supplier Qualification is Needed Before 510k Clearance
Supplier qualification is your 5th priority because you do not want to order all of your prototype parts for the initial testing parts and then find out that the supplier is not capable of supporting you commercially. If you have to switch suppliers you might be forced to repeat biocompatibility testing and other design verification testing due to changes in the manufacturing process. Implementation of a supplier qualification process before 510k clearance is needed.
Label & IFU Requirements Specifications
Label requirements and instructions for use requirements specifications is your 6th priority because you cannot perform electrical safety testing or design validation (including summative usability testing) of your device without labeling and instructions. These requirements are the design inputs for information provided to the user and these must be controlled under design controls rather than document control.
Packaging Specifications
Packaging specifications is the 7th priority you should implement before 510k clearance because the packaging is needed to maintain sterility, to ensure product stability, and to protect the product from shipping. Companies are also frequently surprised by the long lead times associated with ordering custom packaging and you may not have the budget to validate sub-optimal “stock” packaging for your 510(k) submission and then repeat the validation for the optimized packaging later.
Quality System Implementation
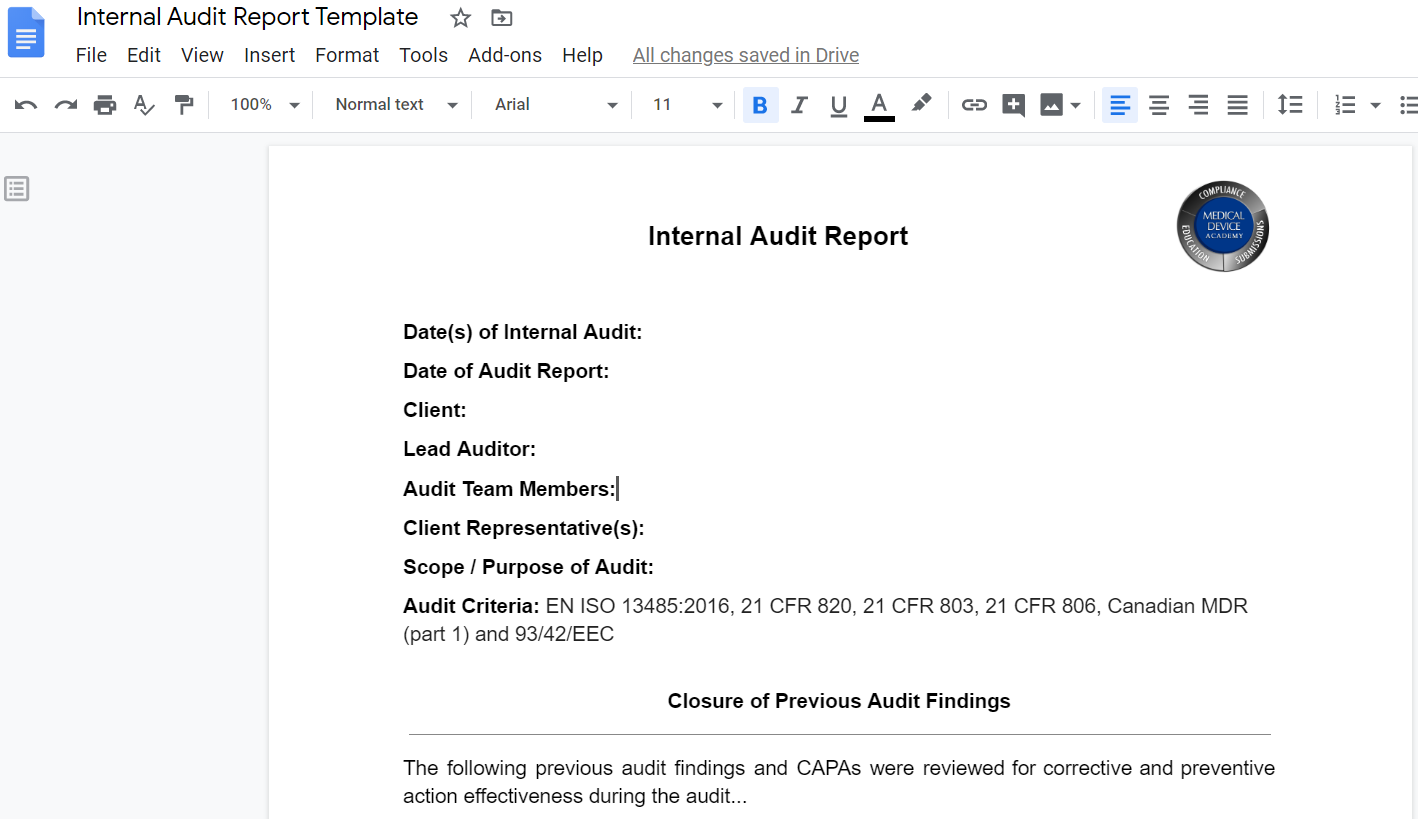
Quality system implementation is the 8th priority for implementation before 510k clearance because you will need a fully functional quality system by the time your 510(k) is cleared. Quality system implementation typically takes 6+ months while the 510(k) review should take 4 months or less. Quality system implementation includes writing 25+ procedures, reviewing and approving those procedures, training your employees, and actually using those procedures to begin generating quality system records. For companies that are pursuing Canadian Licensing or CE Marking, the quality system must be fully implemented and certified before the regulatory submission is possible. (Quality System Requirements for the U.S. FDA are outlined within 21 CFR 820-Quality System Regulation)
Summative Usability Testing
Summative usability testing should happen after Design Freeze or you risk having to backtrack in your design process if this validation test reveals a need for device changes. The FDA’s 2016 Usability Guidance explicitly defines this validation testing as just a portion of overall design validation. (Reference Applying Human Factors and Usability Engineering to Medical Devices Guidance for Industry and Food and Drug Administration Staff (2016))
Apply for Small Business Status Before 510k Clearance
Application for small business status should be the 10th priority for implementation before 510k clearance because this can save your company $16,000+ but it requires that you submit your application at least 60 days before you need to pay the 510(k) user fee.
About the Author
 Matthew Walker – QMS, Risk Management, Usability Testing, Cybersecurity
Matthew Walker – QMS, Risk Management, Usability Testing, Cybersecurity
Matthew came to us with a regulatory background that focused on OSHA and NFPA regulations when he was a Firefighter/EMT. Since we kidnapped him from his other career, he now works in Medical Device Quality Management Systems, Technical/Medical Writing and is a Lead Auditor. He is currently a student in the Champlain College’s Cybersecurity and Digital Forensics program, and we are proud to say that he is also a member of both the Golden Keys and Phi Theta Kappa Honor Societies! Matthew participates as a member of our audit team and has a passion for risk management and human factors engineering. Always the mad scientist, Matthew pairs his professional life in regulatory affairs with hobbies in the culinary arts as he also holds a Butchers/Meat Cutters certificate from Vermont Technical College.
Email: matthew@fdaestar.com
Connect on Linkedin: http://www.linkedin.com/in/matthew-walker-214718101/
Before 510k clearance, 10 quality tasks you need to prevent unexpected delays Read More »