Regulatory Consulting Firm Selection
Things to consider for regulatory consulting firm selection: 1) the project scope, 2) personality, 3) qualifications, and 4) budget.
 Regulatory Consulting Firm Selection
Regulatory Consulting Firm Selection
This article reviews four key considerations of regulatory consulting firm selection. Even if you already have a vice president of regulatory affairs, you still might need external regulatory consulting expertise. Regulatory consultants specialize in just the regulations and most have sub-specialties because it is impossible to know the medical device regulations in every country. Another reason for hiring a regulatory consultant is that you do not have enough bandwidth to conduct the regulatory work internally. Regardless of the scope of the project, this is a strategic decision rather than a tactical one. Regulatory approval impacts your company’s ability to sell devices and therefore a few months of delay can result in a six or seven-figure loss. In addition, the cost of the regulatory consulting fees is likely to be at least five figures. Finally, a purchasing decision of this magnitude will require C-suite approval and your Board of Directors and/or investors may get involved. Here are four critical areas to consider:
1. Defining the scope of the regulatory consulting project
Ensure that the scope, timeline, roles of the consultant/internal company team, and deliverables are crystal clear during consultant interviews and defined within the consulting contract. Do you need advice or suggestions to be carried out by your internal team? Or is “hands-on” work required (writing procedures, conducting training, executing audits, etc.)? I’ve discovered that “hands-on” can mean something entirely different to your company and the consultant. If it’s not clear who is doing the actual work, your internal resources may end up doing the work that was intended for the consultant.
Once the project scope has been clearly explained, ask the prospective consultant to provide a brief document describing how they would approach the project. This will be helpful later on when drawing up the contract. Ask which software or systems the consultant will be using to keep your project on track. A consultant who does not have any version of project management on their laptop, or is unfamiliar with such tools, is a red flag.
Make sure you select a consultant or consulting firm that matches the size of your project. Select and interview three to five companies, based on the size and complexity of the project. If the project primarily involves working at your location, consider the additional cost and travel time from where the consultant(s) is located. If the project allows for working remotely, focus more on the project management aspects mentioned in the previous paragraph, and how your company will communicate with the consultant.
2. Personality of the consultants
When you are making a regulatory consulting firm selection, don’t base your decision on word of mouth, or someone that you pick randomly online. Interviewing is an essential part of the selection process. Be wary of a consultant who talks more than listens, especially if the conversation is about their illustrious career. The consultant you speak with should be focused on the scope of your project and ask questions about your company’s capabilities. You are the client and ultimately your team will be the hero that brings a new medical device to market. The consultant you hire is an experienced guide that has learned from success and failures. Ideally, the consultant will be able to explain the process in simple terms and help you identify critical tasks in the project. Be wary of the consultant that answers every question with “It depends.” If your team’s style of project management and communication doesn’t fit the consulting firm’s style, keep looking.
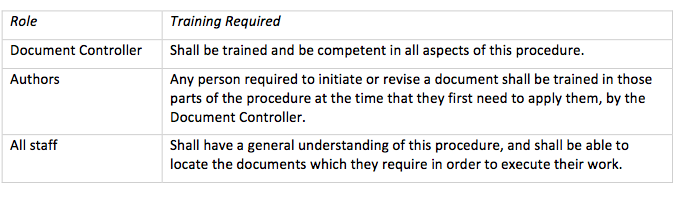
3. Qualifications of the regulatory consulting firm
Don’t limit interviewing to the experience of the lead consultant or owner of the consulting firm. Make sure that you also have a resume or CV for each of the other consulting members that will be working on your project. Imagine the dismay of your internal team when you discover that the owner of the consulting firm has hired friends or former colleagues with little or none of the needed expertise. To prevent this scenario from occurring, include a technical person on the interview team to challenge the expertise of the consultant. This will help you identify a firm that knows all the right buzzwords but lacks the knowledge to accurately implement the deliverables and reduce regulatory risk within your company. Ideally, the consulting firm will have a step-by-step plan and they are able to identify the biggest potential obstacles.
You can ask for and check references for past clients for whom they have done similar work, but people seldom give you the name of a referral that will speak negatively about them. Ask for examples of work reports that the consultant has completed for other clients—with any confidential information removed. This is critical in determining if the final job will be “fluff” or real solutions for your company. It will also avoid the “one size fits all” procedures and processes that can rarely be beneficial for your company’s needs. Ask for examples of “out of the box” thinking and best practices that they’ve implemented. How do they remain current on the regulations and standards?
4. Budget for a regulatory consulting firm
Cost should not be the only determining factor in selecting a consultant. When you’re choosing someone to pave your driveway, you may be able to get away with this. When choosing a regulatory consultant for your medical device company, you want several bids, and you want to ensure that each party is bidding against the same scope and deliverables. However, choosing the least expensive bid over the one with the most expertise and best reputation may cost your company more in the long run if the work isn’t properly done or completed on time.
Contracts must be very specific with regard to milestones, timelines, and deliverables with respect to the payment schedule. What recourse does your company have when a consultant assures you during the interview process that they can meet your every need and then doesn’t? No company wants to have to pay for work that hasn’t been done and may never get done.
If the regulatory consultant is working on-site, be clear about work accommodations – office, cube, conference room, phones, access to printers and company databases, so that there are no misunderstandings once the job starts or excuses for why the work can’t get done “under these conditions.”
Conclusion
Making the best regulatory consultant firm selection is critical. If you are careful in your selection of a regulator consulting firm, you should expect an earlier market launch and a predictable process.
Regulatory Consulting Firm Selection Read More »