DHF Required for a Class I Device? At least 67%…
Is a DHF required appears to be a simple yes/no question? If you reword the question, however, you get a very different answer.
If you ask, “how much less documentation is required for the design of a Class 1 device compared with a Class 2 device?” you get a very different answer. Instead of 0% (Yes, a DHF is required) of 100% (No DHF required), the answer is that you need 33% less documentation for the design of a Class 1 device.
The FDA shared a presentation on design controls in 2015.
In that presentation, the agency identified six Class 1 product classifications that require design controls, while thousands of Class 1 product classifications do not need design controls. Despite the lack of design controls, manufacturers must still maintain a procedure for design transfer, maintain an approved device master file with all the approved design specifications (i.e., design outputs), and design changes may still require revalidation before implementation.
Why is a DHF Required for Class 2, but Not for Class 1?
Class 1 devices are simple devices that are already on the market and have a history of clinical safety. Class 2 devices are generally more complex and present a moderate risk. Therefore, changes in the technological characteristics often present a higher risk for Class 2 devices. When you design a Class 1 device, you still have to determine what your design specifications will be. Again, you don’t need: 1) to review and approve design inputs, 2) a procedure to document your design process, 3) to document formal design reviews, and 4) to create a design plan.
In the 1997 guidance document for design controls, the FDA states that a design transfer procedure should include at least three basic elements:
- design and development procedures should consist of a qualitative assessment of the completeness and adequacy of the production specifications;
- procedures should ensure that all documents and articles which constitute the production specifications are reviewed and approved; and
- procedures should ensure that only approved specifications are used to manufacture production devices.
The first of these basic elements is not required for Class 1 devices because product specifications for most Class 1 devices are simple. The other two requirements are fundamental principles of document control and configuration management. Therefore, you still need a design transfer procedure for Class 1 devices, but you don’t need to include the first element that relies upon design and development procedures.
If you have a Class 1 device, you must still comply with labeling requirements (i.e., 21 CFR 820.120). If your device is sterile, you must still validate and re-validate the process in accordance with 21 CFR 820.75. Class 1 products also require a device master record (DMR) in accordance with 21 CFR 820.181.
What is Not DHF required?
Needed for Class I (67%)
- Approved Design Outputs
- Labeling Procedure
- Approved Labeling
- Sterilization Validation Procedure
- Sterilization Validation Protocol and Report
- Design Transfer Procedure
- Approved DMR
- Design Change Procedure
Needed for Class II and Class I requiring Design Controls (100%)
- Design Control Procedure
- Design Plan
- Approved Design Inputs
- Approved Design Outputs
- Labeling Procedure
- Approved Labeling
- Sterilization Validation Procedure
- Sterilization Validation Protocol and Report
- Design Transfer Procedure
- Evidence of at least 1 Design Review
- Approved DMR
- Design Change Procedure
Therefore, although you do not technically have to have a DHF for a Class 1 products, the difference between the two categories is the following elements:
- Design Control Procedure
- Design Plan
- Approved Design Inputs
- Evidence of at least 1 Design Review
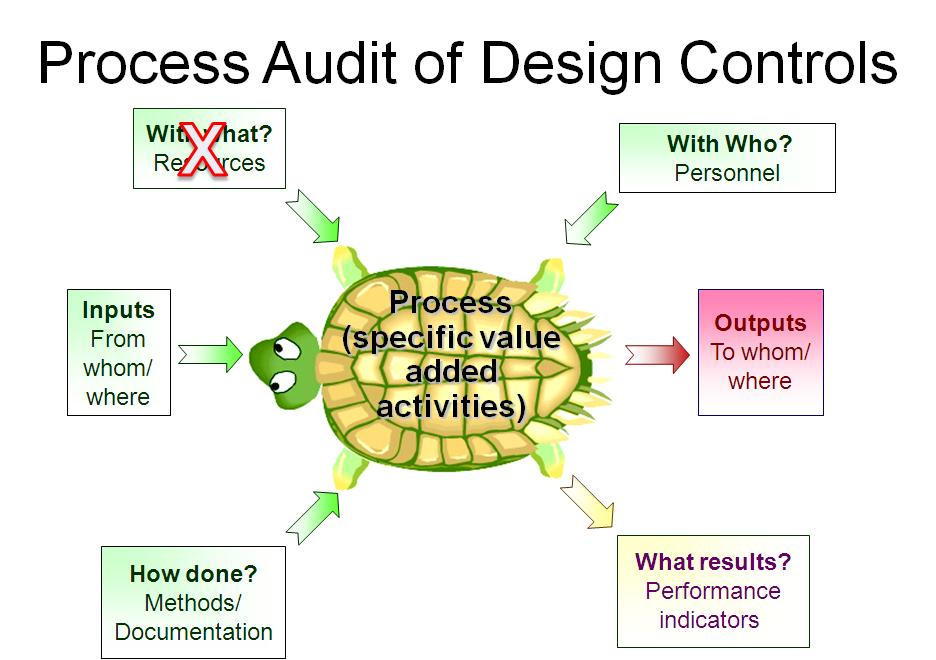
When an FDA inspection occurs, the investigator will review your design control procedure and then audit your DHF in accordance with your design plan.
When you have a Class 1 device, you are not typically inspected unless there is a problem. When ORA inspectors perform an inspection for Class 1 devices, the inspector looks for evidence of items in the first list.
If you are interested in learning more about design history files (DHF), please check out our DHF webinar.
DHF Required for a Class I Device? At least 67%… Read More »