Procedure template for ISO ISO 13485:2016 quality systems
This 12-part procedure template for your medical device QMS can result in writing shorter, more effective documents that facilitate training.
Procedure Template
We all have a standard template for our quality system procedures. Typically, we begin with purpose, scope, and definitions. This 12-part procedure template for your medical device QMS can result in shorter, more effective documents that are easier to train personnel on.
1. Purpose. Often I read something like, “This purpose of this document is to describe the CAPA procedure.” That necessary information is the reason why we title procedures. A better statement of purpose would be, “The purpose of this procedure is to provide a process for identifying, preventing and eliminating the causes of an actual or potential nonconformity, and using risk management principles.” The second version gives readers a better indication of the purpose of the procedure.
2. Scope. This section should identify functions or situations that the procedure applies to, but it is even more critical to identify which situations the procedure does not apply to.
3. References and Relationships. Reference documents that apply to the entire quality management system (e.g., – ISO 13485 and 21 CFR 820) only need to be listed in the Quality Manual. This reduces the need for future revisions to the procedures. I list here any procedure-specific external standard (e.g., – ISO 14971) in the applicable procedure. The relationship between procedures is more important than the references. Therefore, I prefer to use a simple flow diagram, with inputs and outputs, similar to the one below for a document control process.
4. Document Approval. Who must sign off on the procedure? Keep this list short. Ideally, just the primary process owner and Quality Manager (to ensure consistency and integrity across the quality management system).
5. Revision History. A brief listing of each revision and a brief description of what was changed in the procedure.
6. Responsibilities and Authorities. A listing of the main areas of responsibility for each role. Remember to include the title of managers who may be required to approve forms, or make key decisions.
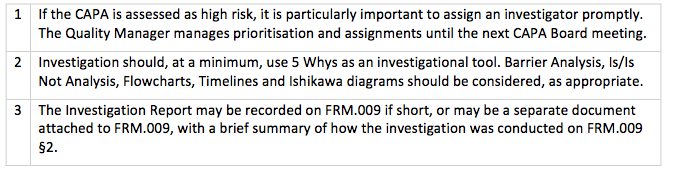
7. Procedure. I prefer to create a detailed flowchart outlining each step of a process before writing the procedure. Each task box in the flowchart will include a reference number. If you organize the reference numbers in an outline format, then you can write the text of your procedure to match the flowchart—including the numbering of the flowchart task boxes.
8. Monitoring and Measurement. An explanation of how the process is monitored and measured, who does it, how often, format, method of communicating the analysis, and what process that analysis will be input into, e.g., Management Review.
9. Training/Retraining. Tabulated, which roles need to be trained in this procedure, and to what level? The example below is also from a Document Control procedure.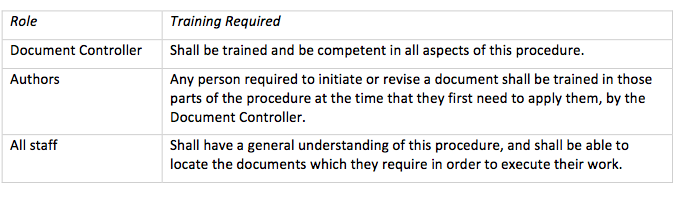
10. Risk Management. This section identifies risks associated with each procedure and how the procedure controls those risks. As well as complying with the requirement to apply risk management throughout product realization (i.e., Clause 7 of ISO 13485), including a section specific to risk management forces the author of the procedure to think of ways the process can fail and to develop ways to avoid failure. Risks can also be a starting point for training people on the procedure.
11. Records. Tabulated, form number and names, a brief description of its purpose, and a column for retention and location. This column also allows for reference to compilations if the record becomes part of, e.g., the Design History File, Device Master Record, or the Risk Management File.
12. Flowcharts. Step-by-step through the process, saying who performs the step when it isn’t apparent. I keep task shapes simple: rectangles for tasks, rounded rectangles for beginnings and endings, diamonds for decision boxes, and off-page reference symbols.
When the task needs supporting text, e.g., guidance or examples, put a number in the box and a corresponding number in the table in (7) above. Ideally, the flowcharts are placed in the document with the Notes table on the same page or the opposite page. In practice, I often put them at the end to simplify the layout. One of my clients loves her flowcharts and puts them on the front page.
Benefits of this Approach
Information is well structured and presented consistently across procedures, more so than can be achieved through narrative.
- The flowchart is the primary means of documenting the procedure.
- Tables provide details that are not clear in the flowchart.
The procedure structure described above facilitates a consistent training approach built around the document. Purpose and scope are presented first, and then the Risk section is presented to explain what is essential in the procedure and why. The flowchart, the table, and the formwork together describe each step of the procedure. Finally, a PowerPoint template can be used to guide process owners in developing their training.
And to make it even easier, you have already spelled out who needs to be trained and to what level.
Procedure template for ISO ISO 13485:2016 quality systems Read More »


 If your company needs help with IEC 60601-1 gap analysis, preparation of the risk management file for the third edition, or training on the Standard, please
If your company needs help with IEC 60601-1 gap analysis, preparation of the risk management file for the third edition, or training on the Standard, please 







